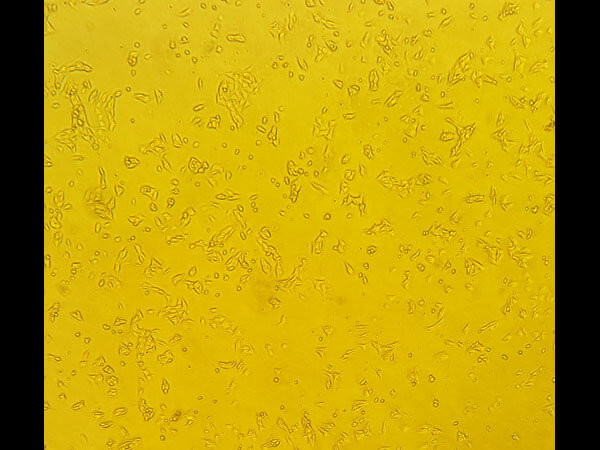
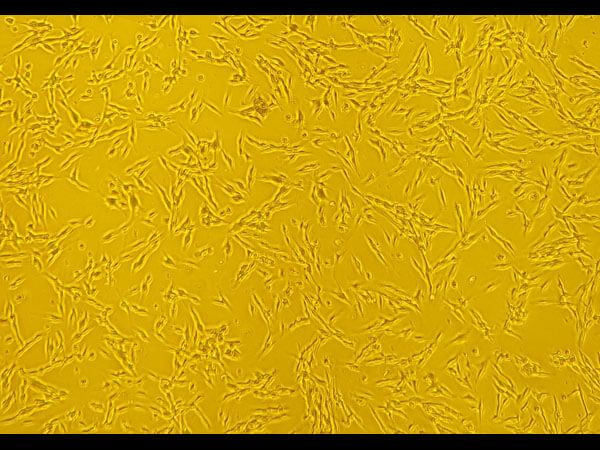
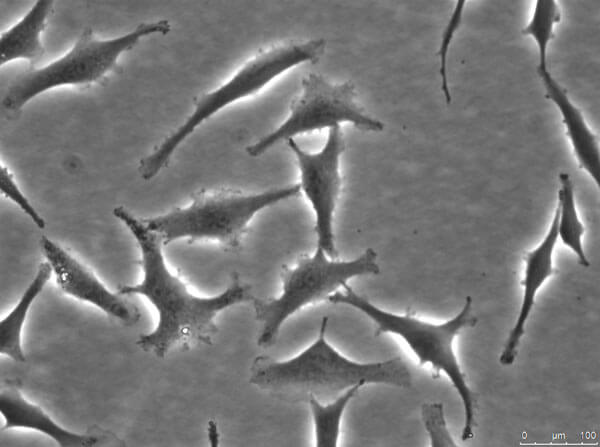
Cell Lines
Rockland's Cell Lines category is a pivotal resource for researchers aiming to unveil critical target genes and pathways influenced by genomic alterations, enhancing the precision of predictions regarding the efficacy of novel cancer therapeutics. Through our collaboration with the Wistar Research Institute, we offer an extensive panel of low-passage human melanoma cell lines derived from freshly excised metastases, meticulously produced, validated, and distributed to support your melanoma cancer research endeavors.
- Clinical predictability: Stable in gene expression, architecture, and mutation status
- Genetic characterization: Profiled for BRAF, N-RAS, KIT, PTEN, and CDK4 mutations
- Research versatility: Ideal for genetic studies, drug testing, and more
Product Categories